How to Treat Low Testosterone in Women: Treatment Options
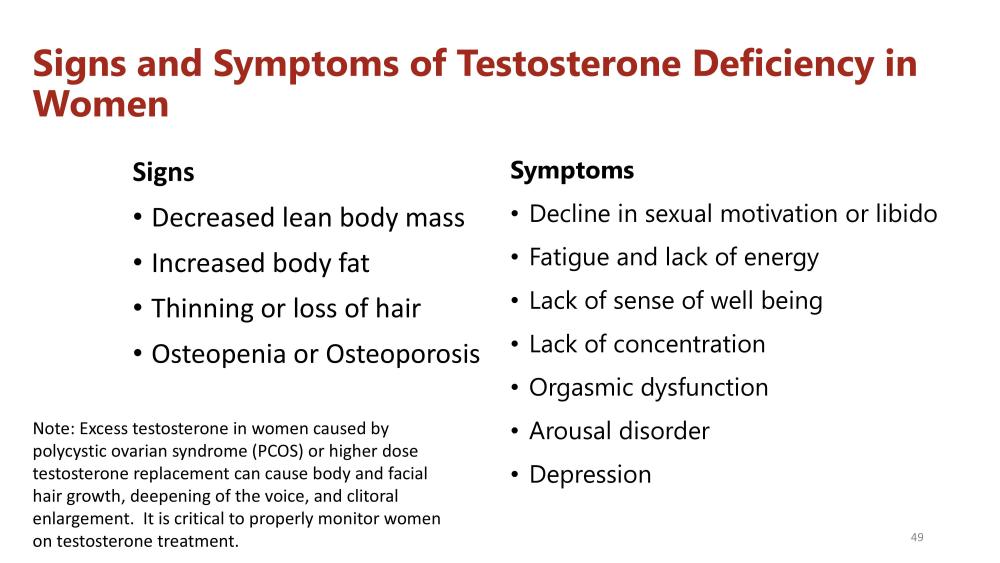
Testosterone is typically thought of as a hormone for men. Still, it is also essential for women as it influences sexual functioning, mood, the development of lean muscle mass, and even memory and cognition. Women who are in their 40s have about half the level of testosterone that was present in their 20s. We see a significant decline in testosterone levels over time. Women with low or suboptimal testosterone levels can experience many symptoms, including sexual dysfunction and a decrease in sexual drive or desire, known as low sex drive (hypogonadism). They can also notice that they have increased fatigue. They're tired. Also, it's more challenging to develop lean muscle mass. It can have a significant impact even on mood, an overall sense of well-being, motivation, a feeling of confidence, and assertiveness. Also, it can affect memory and cognitive function. A low libido: As testosterone helps fuel a healthy sex drive, a decline in sexual interest or inability to achieve orgasm may be a symptom of lower testosterone levels in both sexes.
A study published in the journal of the American Medical Association showed that approximately 43% of postmenopausal women suffer from some form of sexual dysfunction. Surprisingly, we don't hear a lot about this condition in women. We certainly don't hear about options for treatment, including testosterone. This condition can often go undiagnosed and undertreated.
NO FDA-APPROVED TREATMENTS FOR LOW TESTOSTERONE ON WOMEN
Currently, there is no FDA-approved testosterone replacement therapy for women, even though providers have been prescribing it in an off-label manner, which is when a medication is prescribed for something other than its official FDA-approved indication. Providers have been doing this for over 50 years now. Testosterone can be replaced in various forms. It can be given in a shallow-dose injection once a week. It can also be given sublingually in a troche form, which dissolves in the mouth. Also, it can be administered through a minor surgical procedure. It's known as subcutaneous pellet insertion. And then it can also be given in topical form as a cream or a gel.
The most common form of replacement we see is topical gel or cream, which can be supplied by compounding pharmacies. The benefit of doing it this way is that the provider can adjust the dose based on the individual patient's needs and response to therapy. It's more than just one standard dose, and it better work for you, or there's no other option. Testosterone creams can be customized for the needs of the individual patient. When you replace any hormone in this manner at low daily doses, it is very similar to the way the body naturally produces hormones.
After starting testosterone replacement therapy, women typically notice a significant improvement in all symptoms, including increased sexual functioning, desire, and drive. They can also see an increase in energy levels and an increased ability to develop lean muscle mass. Additionally, they can notice a significant improvement in mood, motivation, overall sense of well-being, and confidence. In addition, they may see improved memory and cognitive functioning.
Another critical point is that when testosterone is given to a woman, a portion of it will convert to estrogen. The postmenopausal woman with low estrogen levels can see improvement in those symptoms typically associated with low estrogens, such as hot flashes, night sweats, moodiness, irritability, and vaginal dryness. So, women may experience improvements in the classic symptoms of low testosterone and the typical menopausal symptoms associated with low estrogen.
Several studies support the use of hormone replacement therapy, specifically testosterone replacement therapy, in women. A Cochrane review of the literature found that over 35 trials have been performed, which included over 4500 women. They found a significant improvement in sexual functioning in women on hormone replacement therapy. Also, a more recent study published in 2014 showed that women on a transdermal or topical form of hormone replacement therapy had an improvement in memory and cognitive functioning. Several studies support the use of this vital hormone in women.
POTENTIAL SIDE EFFECTS OF TESTOSTERONE IN WOMEN
In terms of safety, there are potential side effects with the use of any medication. In testosterone therapy, if doses are too high, women can notice adverse effects, such as acne and an increase in hair growth, known as hirsutism. Also, with extremely high doses, they may see a deepened voice or enlargement of the labia or clitoris. That would typically be something that's dose-dependent. If a physician was a little bit aggressive with their starting dose, they might notice some side effects of testosterone treatment, such as disturbed breathing while sleeping, breast swelling or tenderness, swelling in the ankles, or too much testosterone. Doctors also watch out for high red blood cell counts, which could increase the risk of clotting. By decreasing and backing off on the dosage, those symptoms will resolve.
One important fact to mention for premenopausal women who are still menstruating is that providers need to discuss the use of birth control with them because testosterone is considered category X, meaning it will cause fetal harm if a woman becomes pregnant while she's on testosterone replacement. That's just a discussion that the patient needs to have with their provider, “What is your reliable form of birth control?" before prescribing it to them. Testosterone replacement therapy is very safe for premenopausal women on birth control and postmenopausal women. It has a low risk of side effects when used at appropriate doses, and many studies support its use in this population.
SEXUAL DYSFUNCTION AND LOW TESTOSTERONE IN WOMEN
We are all aware that if we watch TV for more than an hour each day, we will constantly see advertisements for medications to treat erectile dysfunction in men. But we hardly hear anything about sexual dysfunction in women. There are many reasons why women’s sexual desire and other hormone-related quality-of-life issues are so misunderstood, underdiagnosed, and undertreated.
Sexual dysfunction in pre and post-menopausal women has been a very controversial topic that has been poorly researched, even though a February 1999 study published in the Journal of the American Medical Association, titled “Sexual Dysfunction in the United States: Prevalence and Predictors,” found that approximately 43% of postmenopausal women suffer from some form of female sexual dysfunction.
It wasn’t until June 2011 that an FDA advisory committee to the division of Reproductive and Urologic Drug Products stated that HSDD (Hypoactive Sexual Desire Syndrome) is a significant medical condition for women. This may open the door for companies to apply for new drug applications for that indication.
It is important to note that unlike erectile dysfunction drugs approved for men, like Viagra, which increase blood flow to the genitals as long as a man is aroused, testosterone therapy is systemic and needs to be applied over weeks to have a noticeable effect on sex drive in men and women.
Some companies have tried to enter the female sexual dysfunction market in the past. In December 2004, the United States FDA rejected Procter & Gamble's fast-track request for Intrinsa (a testosterone patch for women) for HSDD, citing concerns about potential off-label use of the product. In Canada, post-menopausal women have been able to obtain government-approved testosterone treatment since 2002. In 2007, Intrinsa was granted a license from the European Medicines Agency in July and was available on Britain's National Health Service.
According to P&G's survey on female health, 30 million women in the U.S. are naturally menopausal, 3 million are distressed by their lack of sexual desire, and 20% of 25 million surgically menopausal women are distressed.
Other companies that attempted to get their drugs approved for this indication (Boehringer Ingelheim and Warner Chilcott) have pulled the plug on their competing HSDD treatments for menopausal and pre-menopausal women.
BioSante Pharmaceuticals also got their testosterone gel for women, LibiGel, rejected by the FDA.
HORMONE THERAPY IN POSTMENOPAUSAL WOMEN
Menopause can cause symptoms such as hot flashes that might result from the changing hormone levels during the menopause transition. After a woman's last menstrual period, when her ovaries make much less estrogen and progesterone, some symptoms of menopause might disappear, but others may continue.
To help relieve these symptoms, some women use hormones. This is called hormone therapy (HT), which includes estrogen alone or in combination with progesterone. HT is available orally or in gel formulations made by specialized compounding pharmacies.
Estrogen is a hormone used to relieve the symptoms of menopause. A woman who had her uterus removed could use only estrogen (E). But a woman with a uterus must add progesterone, or progestin (synthetic progesterone), and estrogen (E+P). This combination lowers the chance of an unwanted thickening of the uterus lining and reduces the risk of cancer of the uterus, an uncommon but possible result of using estrogen alone.
CONTROVERSIES IN HORMONE TREATMENTS FOR WOMEN
But the use of hormone therapy in women has been subject to much controversy in the recent past.
The Women's Health Initiative (WHI) was a landmark clinical trial that looked at the effects of combination hormone therapy (estrogen + progestin) in 16,608 postmenopausal women with an intact uterus. The women were aged 50 to 79 (average age of 63) when they joined the study. This study did not include the use of testosterone. In this study, 8,506 participants were randomly assigned to receive a combination of estrogen (0.625 milligrams of conjugated equine estrogens per day) plus progestin (2.5 mg of medroxyprogesterone acetate), and 8,102 women were given a placebo.
The study was stopped in 2002 after an average of 5.6 years of treatment due to increased breast cancer in women on hormone therapy. Compared to women on placebo, women on combination hormone therapy were also at increased risk of stroke, dangerous blood clots, and heart disease. In contrast, their risk of colorectal cancer and hip fractures was lower.
It is important to note that these hormones were provided orally, and some clinicians claim that transdermal (on the skin) application of estrogen alone or in combination with testosterone would show a different and more favorable side effect profile.
The halting of the WHI study raised concerns about the safety of all hormone therapy in women (oral or transdermal), even if no androgens were included in this study and only oral delivery forms were used. Many physicians stopped prescribing hormone therapy (HT) even for women who had dramatic improvements in their quality of life while using it. Experts today don't recommend hormone therapy unless a woman suffers painful menopause symptoms.
New information about the use of androgens (testosterone and DHEA) alone or with HT suggests that these hormones may help women who do not have enough androgens and have problems with their sexual health.
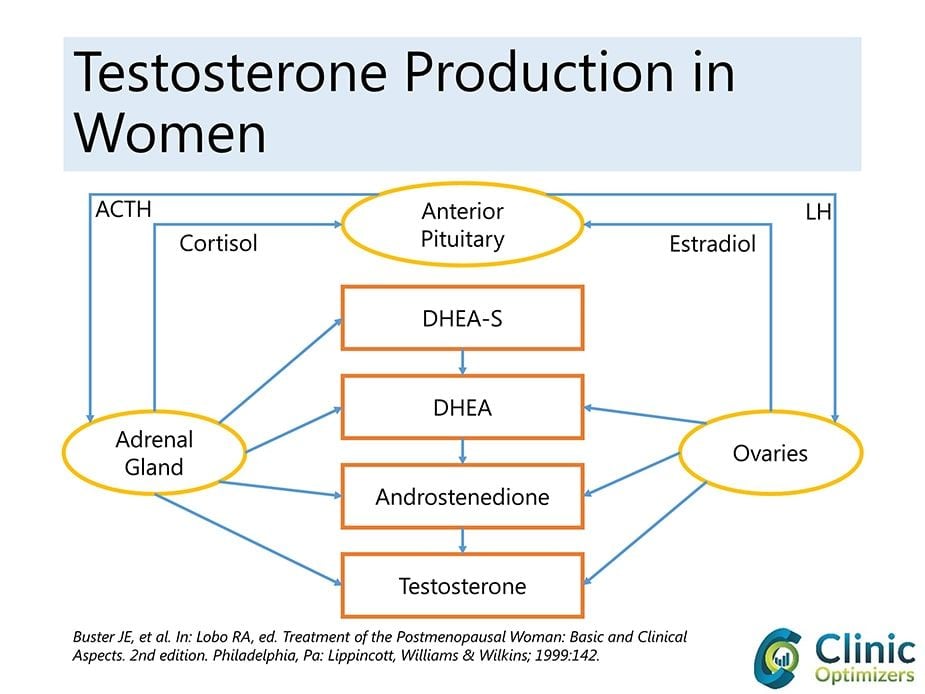
Androgens are also precursors of all estrogens (estrone (E1), estradiol (E2), and estriol (E3)) in women's bodies. The primary and most well-known androgen is testosterone (which aromatizes into estradiol); other less essential androgens are dihydrotestosterone (DHEA) and androstenedione. The ovaries and adrenals directly secrete androgens in women.
Presently, there is no agreement about whether androgen deficiency is a clinical problem in aging women and if the addition of androgens to HT can improve the cardiovascular risks seen in the WHI study.
Causes of androgen insufficiency in women can have ovarian, adrenal, hypothalamic-pituitary, drug-related, and unknown origins. Symptoms of adrenal insufficiency and androgen insufficiency in women may include a diminished sense of well-being, low mood, fatigue, and hypoactive sexual desire disorder (HSDD) with decreased libido or reduced sexual receptivity and pleasure that causes a great deal of personal distress. Premature ovarian insufficiency (POI) is another possible cause of androgen insufficiency in women. POI occurs when the ovaries stop functioning normally before 40 years of age. Although menopause is the most common cause of ovarian failure, other factors, such as chemotherapy or radiation therapy, can also contribute to POI. Therefore, it is important to consider premature ovarian insufficiency as a potential cause of androgen insufficiency in women.
There is increasing evidence to suggest that many postmenopausal women experience symptoms alleviated by androgen therapy and that such symptoms may be caused by androgen deficiency. Affected women complain of fatigue, low libido, and diminished well-being, which are symptoms easily and frequently attributed to psychosocial and environmental factors.
The question of whether adding testosterone therapy to conventional postmenopausal HT is effective or safe is unresolved. Therefore, a Cochrane review was performed to determine the efficacy and safety of testosterone therapy for postmenopausal women using HT. Thirty-five trials with a total of 4768 participants were included in the review. The median study duration was six months (range: 1.5 to 24 months). Most of the trials were of adequate quality regarding randomization. The pooled estimate suggested that adding testosterone to HT regimens improved sexual function scores and the number of satisfying sexual episodes for postmenopausal women. Some of the few adverse effects were decreased high-density lipoprotein (HDL) cholesterol levels and increased hair growth and acne incidence. The discontinuation rate was not significantly higher with the addition of testosterone therapy.
OTHER USES FOR TESTOSTERONE IN WOMEN
Emerging and controversial potential indications for androgen therapy in women have been or are being evaluated. Women with early ovarian failure, premenopausal androgen deficiency symptoms, postmenopausal and glucocorticosteroid-related bone loss, HIV-related wasting, and the premenstrual syndrome can all use this medicine. Whether or not any of these indications will lead to approved products in the future is unknown.
HOW TO MEASURE LOW TESTOSTERONE IN WOMEN
The term hypogonadism is used as a diagnostic term for testosterone deficiency, also known as testosterone insufficiency, in men. Besides HSDD as one of the potential symptoms, there is no agreement on what to call androgen deficiency in women. Clinical guidelines published in 2002 called the Princeton Consensus Statement used the term "female androgen insufficiency" as defined as a pattern of clinical symptoms in the presence of decreased bioavailable testosterone and normal estrogen status.
The panel warned that currently available testosterone assays were found to lack sensitivity and reliability at the lower testosterone blood level ranges in women. The need for an equilibrium dialysis measure was strongly emphasized as the most adequate method to test women’s testosterone blood levels.
BUY THE MOST AFFORDABLE AND ACCURATE TESTOSTERONE TEST FOR WOMEN
Women in the United States can buy a testosterone test for women online without needing a doctor's prescription by using DiscountedLabs.com. They can also obtain a complete blood test panel to measure other hormones like estrogen, DHEA, progesterone, and testosterone.
HOW TO TREAT LOW TESTOSTERONE IN FEMALES
Circulating testosterone in women declines during the late reproductive years, such that otherwise healthy women in their 40s have approximately half the testosterone level as women in their 20s. The levels remain stable across the menopausal transition and then either remain stable or continue to decline with diminishing adrenal androgen production with increasing age. In the decade preceding menopause, the mid-cycle surge of free testosterone is lost. Despite this, research showing the benefits of androgen replacement has been limited to postmenopausal years. This means that testosterone levels in women change throughout the month based on one's menstrual cycle. However, the mid-cycle surge of free testosterone is lost in the decade preceding menopause.
Some small studies have been done in premenopausal women, however. One evaluated the efficacy of transdermal testosterone therapy on mood, well-being, and sexual function in premenopausal women with low libido in eugonadal (normal testosterone blood levels). Testosterone therapy improved the well-being, mood, and sexual function of these women. Since many women experience diminished sexual interest and welfare during their late reproductive years, further research is warranted to evaluate the benefits and safety of the longer-term intervention. Potential dose-dependent side effects may be unwanted hair growth, masculinization, and high-density lipoprotein (HDL) lowering.
TESTOSTERONE REPLACEMENT AND CARDIOVASCULAR RISKS IN WOMEN
A direct association between testosterone and heart disease has never been established, but doctors have suspected a link exists for many years. The reasoning goes like this: men have much more testosterone than women and develop heart disease about ten years before their female counterparts.
On top of standard medical therapy, women with systolic heart failure who took low-dose testosterone for six months showed significant gains in exercise and ventilatory capacity and large-muscle strength, along with heightened insulin sensitivity, in a small placebo-controlled trial .
Despite the entrenched belief that higher blood levels of testosterone increase the risk of CVD in women, data from recent observational studies mostly show an inverse relationship between testosterone and CVD risk. A pilot study (JCEM 86 (1): 158) suggested favorable effects of transdermal testosterone treatment of women with established congestive cardiac failure, which merits further evaluation. Some early research shows that giving postmenopausal women testosterone therapy through injections improves both flow-mediated and GTN-mediated vasodilation in the brachial artery. The mechanisms underlying these potentially beneficial cardiovascular effects require further investigation.
TESTOSTERONE REPLACEMENT AND CANCER IN WOMEN
The relationship between endogenous testosterone production and breast cancer risk remains contentious, with recent studies indicating either no relationship or a possible increase in risk when estrone and estradiol are not considered. No randomized controlled trial of testosterone therapy has been sufficiently large or of sufficient duration to establish whether such treatment may influence breast cancer occurrence. There does not appear to be an association between testosterone and endometrial cancer or other malignancies in the review of published studies.
There is no convincing evidence that standard estrogen-based hormone therapy for ovarian failure increases the risk of breast cancer. However, some studies have previously shown that ovarian androgens protect mammary epithelial cells from excessive estrogenic stimulation. Therefore, a study hypothesized that adding testosterone to usual hormone therapy might protect women from breast cancer. This retrospective observational study followed 508 postmenopausal women receiving testosterone and standard hormone therapy in South Australia. Breast cancer status was ascertained by mammography at the initiation of testosterone treatment and biannually after that. The average age at the start of follow-up was 56.4 years, and the mean duration of follow-up was 5.8 years. Breast cancer incidence in this group was compared with that of untreated women and women using usual hormone therapy reported in the medical literature and to age-specific local population rates.
There were seven cases of invasive breast cancer in this population of testosterone users, for an incidence of 238 per 100,000 woman-years. The rate for estrogen/progestin and testosterone users was 293 per 100,000 woman-years—substantially less than women receiving estrogen/progestin in the Women's Health Initiative study (380 per 100,000 woman-years) or the Million Women Study (521 per 100,000 woman-years). The breast cancer rate in testosterone users in this study was closest to that reported for users who never used hormone therapy in the latter study (283 per 100,000 woman-years), and their age-standardized rate was the same as for the general population in South Australia.
Based on these findings, adding testosterone to traditional hormone therapy for postmenopausal women may not raise the risk of breast cancer and may even lower it, bringing the rates back to what they are in the general population that is not on hormone therapy. But more studies are needed.
LATEST DATA ON TESTOSTERONE AND WOMEN:
A recent study review by Dr. Rakibul Islam and his team was published in The Lancet in July 2019 and retrieved 46 reports of 36 randomized controlled trials comprising 8480 female participants. Their meta-analysis showed that testosterone significantly improved sexual function compared to a placebo or a comparator (e.g., estrogen with or without progesterone). It improved sexual desire, pleasure, arousal, responsiveness, and self-image, and it decreased sexual concerns and distress in postmenopausal women. A significant rise in the amount of LDL-cholesterol and reductions in total cholesterol, HDL-cholesterol, and triglycerides were seen with testosterone administered orally but not when administered non-orally (e.g., by transdermal patch or cream). An overall increase in weight was recorded with testosterone treatment. No effects of testosterone were reported for body composition, musculoskeletal variables, or cognitive measures, although the number of women who contributed data for these outcomes was small. Testosterone was associated with a significantly greater likelihood of reporting acne and hair growth, but no serious adverse events were recorded.
TESTOSTERONE USE IN WOMEN IN THE UNITED STATES
As previously mentioned, there is no FDA-approved testosterone product for women. Some doctors prescribe drugs for female patients by having them use low doses of products like Androgen, Testim, Axiron, Testopel, and Fortesta that are meant for male hypogonadism without following the product's label. Other doctors prescribe creams with low testosterone levels through compounding pharmacies. However, it is important to note that women and people with AFIB require significantly less testosterone, necessitating a much lower dose of medication compared to men.
CONCLUSION
In conclusion, low testosterone in women is a condition that is often overlooked and underdiagnosed. However, it can have significant impacts on a woman's quality of life, including decreased sex drive, fatigue, and mood changes. Fortunately, there are several treatment options available, including hormone replacement therapy, lifestyle changes, and medication. It is important for women to speak with their healthcare provider and get properly diagnosed and treated for low testosterone if necessary. By doing so, they can improve their overall health and well-being.
References:





