The Underestimated Risks of Low Testosterone Levels: A Comprehensive Guide
Testosterone is more than just a sex hormone. It plays a crucial role in a range of physiological processes, including the development of muscle mass, bone density, and even the modulation of blood sugar levels. While high levels of testosterone can have their own set of complications, this article focuses on the often-underestimated risks associated with low testosterone levels.
What is Low Testosterone?
Low testosterone is a condition where the body does not produce sufficient amounts of the hormone. The threshold for low testosterone varies, but it is generally considered to be below 300 ng/dL (nanograms per deciliter) for adult men. The condition can lead to various health issues, ranging from metabolic syndrome to increased risk of death from all causes.
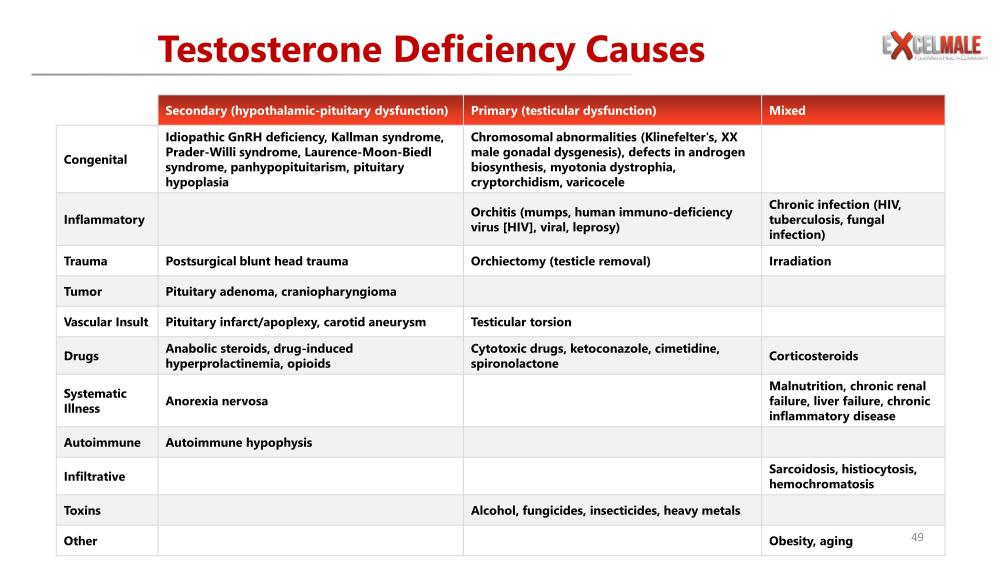
Understanding the Causes of Low Testosterone:
Testosterone, the primary male sex hormone, plays a crucial role in maintaining a range of bodily functions, from muscle mass and fat distribution to bone density and red blood cell production. While it's common for testosterone levels to decline as men age, significantly low levels can lead to a host of health issues. But what causes low testosterone levels? The reasons are many and can range from genetic conditions to lifestyle choices. Let's break it down.
Secondary Causes: Hypothalamic-Pituitary Dysfunction
Idiopathic GnRH Deficiency, Kallman Syndrome, and More
Sometimes, low testosterone can be due to issues with the pituitary gland or the hypothalamus, parts of the brain that signal the testicles to produce testosterone. Conditions such as Idiopathic GnRH deficiency and Kallman syndrome can disrupt these signals. These conditions are examples of hypogonadotropic hypogonadism (Bhasin et al., 2010).
Inflammatory Causes
Inflammation of the pituitary gland can also result in low testosterone. This inflammation can be due to a variety of factors, including autoimmune reactions and certain illnesses (Dandona & Rosenberg, 2010).
Trauma and Tumors
Blunt head trauma or postsurgical complications can affect the pituitary gland, leading to low testosterone. Tumors like pituitary adenomas or craniopharyngiomas can have similar effects (Wu et al., 2010).
Vascular Insult
Issues with the blood vessels that supply the pituitary, such as pituitary infarct/apoplexy or carotid aneurysm, can also be a culprit.
Drug-Induced Causes
Certain medications like anabolic steroids, opioids, and drugs that induce hyperprolactinemia can contribute to low testosterone. Always consult your doctor if you are on medication and experiencing symptoms of low testosterone (Bhasin et al., 2010).
Systematic Illness and Autoimmune Causes
Chronic illnesses such as anorexia nervosa, chronic renal failure, and liver failure can result in low testosterone. Autoimmune conditions that attack the pituitary gland (autoimmune hypophysis) can also be a factor (Dandona & Rosenberg, 2010).
Primary Cause: Testicular Dysfunction
Chromosomal and Genetic Factors
Issues right at the level of the testicles can also be causes. Conditions like Klinefelter's syndrome, XX male gonadal dysgenesis, and defects in androgen biosynthesis are all chromosomal abnormalities that can lead to low testosterone (Wu et al., 2010).
Infections and Surgeries
Orchitis (inflammation of the testicles due to infections like mumps or HIV) and orchiectomy (surgical removal of the testicle) can directly affect testosterone production.
Other Factors
Chronic infections like tuberculosis, irradiation, testicular torsion, and certain medications can also be responsible.
Lifestyle and Other Factors
Factors like obesity, aging, malnutrition, and exposure to toxins such as heavy metals and alcohol can also influence testosterone levels (Dandona & Rosenberg, 2010).
Low testosterone can result from a variety of causes, ranging from medical conditions and medications to lifestyle choices. If you're experiencing symptoms, it's crucial to consult a healthcare provider for a comprehensive diagnosis and treatment plan.
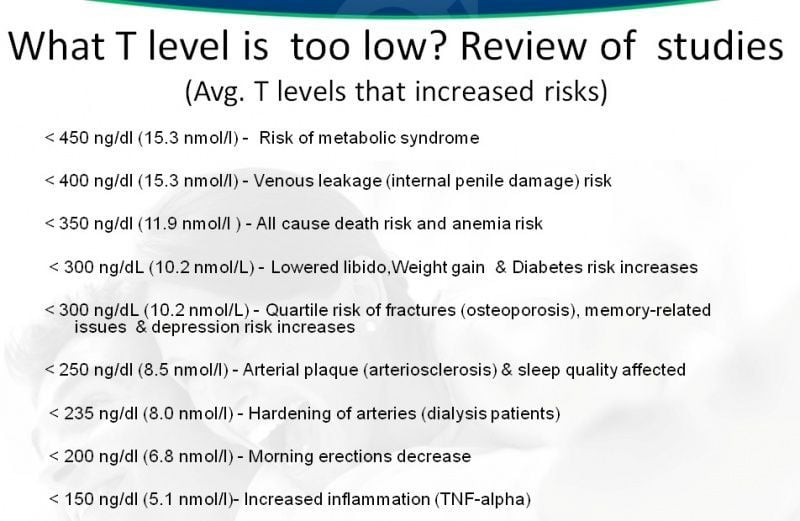
Risks Associated with Different Levels of Low Testosterone
< 450 ng/dl (15.3 nmol/l) - Risk of Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that include high blood pressure, elevated blood sugar levels, excess body fat, and abnormal cholesterol levels. Testosterone plays a significant role in regulating these physiological functions. Research by Dhindsa et al. has highlighted the increased risk of metabolic syndrome in men with testosterone levels below 450 ng/dl1.
< 400 ng/dl (15.3 nmol/l) - Venous Leakage (Internal Penile Damage) Risk
Venous leakage is a condition that can result in erectile dysfunction due to internal penile damage. According to a study by Yassin and Saad, men with testosterone levels below 400 ng/dl are at a higher risk of developing this condition2.
< 350 ng/dl (11.9 nmol/l) – All-Cause Death Risk and Anemia Risk
Khaw et al. conducted a study that showed men with testosterone levels below 350 ng/dl had an increased risk of death from all causes, as well as a higher risk of developing anemia3.
< 300 ng/dL (10.2 nmol/L) - Lowered Libido, Weight Gain & Diabetes Risk Increased
A low level of testosterone can also have a detrimental effect on sexual health, including a decrease in libido. Furthermore, it is associated with weight gain and an increased risk of developing diabetes. Traish et al. discussed these risks in their research4.
< 300 ng/dL (10.2 nmol/L) - Quartile Risk of Fractures (Osteoporosis), Memory-Related Issues & Depression Risk Increases
Testosterone is crucial for bone density. Low levels can increase the risk of fractures, memory-related issues, and even depression. A study by Orwoll et al. emphasized these risks5.
< 250 ng/dl (8.5 nmol/l) - Arterial Plaque (Arteriosclerosis) & Sleep Quality Affected
Vlachopoulos et al. found that men with testosterone levels below 250 ng/dl had a higher risk of developing arterial plaque, which can lead to arteriosclerosis. Additionally, these men experienced a reduction in sleep quality6.
< 235 ng/dl (8.0 nmol/l) - Hardening of Arteries (Dialysis Patients)
Carrero et al. identified that low testosterone levels can increase the mortality risk among male dialysis patients by promoting the hardening of arteries7.
< 200 ng/dl (6.8 nmol/l) - Morning Erections Decrease
A study by O'Connor et al. showed that men with testosterone levels below 200 ng/dl experienced a decrease in morning erections, which is often a sign of erectile dysfunction8.
< 150 ng/dl (5.1 nmol/l) - Increased Inflammation (TNF-alpha)
Malkin et al. found that extremely low levels of testosterone, under 150 ng/dl, were associated with increased inflammation markers like TNF-alpha9.
Conclusion
Low levels of testosterone are linked to a wide range of health issues. While testosterone replacement therapy is often recommended for men with low levels, understanding the risks associated with varying degrees of low testosterone is crucial for effective treatment and prevention. Always consult your healthcare provider for diagnosis and treatment.
Buy a Low Cost Total and Free Testosterone Test on DiscountedLabs.com:
Low Testosterone: What Do Different Medical Guideline Groups Say?
Understanding the guidelines for diagnosing and treating low testosterone is crucial for both healthcare providers and patients. Different medical organizations have released various guidelines over the years, making it essential to know how each defines low testosterone levels. This article aims to shed light on what various medical guideline groups have to say about low testosterone, focusing on cutoff values and expert opinions.
Expert Opinion
Before delving into specific guidelines, it's worth noting that expert opinion often plays a significant role in forming these guidelines. Medical professionals and researchers contribute to these guidelines based on clinical experience, existing studies, and ongoing research. Therefore, guidelines are not static but evolve over time, reflecting the current state of medical knowledge.
Year of Release and Update
Knowing when a particular guideline was released or updated is important as it indicates the currency and relevancy of the information. Here is a brief timeline:
- ISSAM: 2005
- Endocrine Society: 2006
- ISSM: 2008
- AUA: 2015
- ICSM: 2015, updated in 2018
Cutoff Values of Testosterone for Laboratory Diagnosis
One of the most critical aspects of diagnosing low testosterone is determining the cutoff values. Various organizations have different parameters. Here's a summary:
| Guideline Group | Cutoff Values for Total T (TT) | Cutoff Values for Free T | Year |
|---|---|---|---|
| ISSAM | TT < 231 ng/dL (8 nmol/L) | N/A | 2005 |
| Endocrine Society | TT: 231-346 ng/dL (8-12 nmol/L) | Free T < 52 pg/mL | 2006 |
| ISSM | TT < 230 ng/dL (8 nmol/L) | Free T < 52 pg/mL | 2008 |
| AUA | TT: 230-350 ng/dL (8-12 nmol/L) | Free T < 65 pg/mL | 2015 |
| ICSM | TT < 300 ng/dL | Free T < 5 ng/dL | 2018 |
Definitions and Abbreviations:
- ISSAM: International Society for the Study of the Aging Male
- ISSM: International Society for Sexual Medicine
- ICSM: International Consultation for Sexual Medicine
- AUA: American Urological Association
- TT: Total Testosterone
- Free T: Free Testosterone
- SHBG: Sex Hormone-Binding Globulin
Understanding the various guidelines for diagnosing low testosterone is crucial for appropriate treatment. It's evident that different medical organizations have varying cutoff values, and these may be subject to change as more research becomes available. Always consult your healthcare provider for the most current and personalized advice.
By keeping updated on these guidelines, both physicians and patients can make more informed decisions regarding the diagnosis and treatment of low testosterone.
Sources:
- International Society for the Study of the Aging Male (ISSAM), Guidelines, 2005.
- Endocrine Society, Clinical Guidelines, 2006.
- International Society for Sexual Medicine (ISSM), Guidelines, 2008.
- American Urological Association (AUA), Guidelines, 2015.
- International Consultation for Sexual Medicine (ICSM), Guidelines, 2015, updated in 2018.
Footnotes
-
Dhindsa, S., Miller, M. G., McWhirter, C. L., Mager, D. E., Ghanim, H., Chaudhuri, A., & Dandona, P. (2010). Testosterone concentrations in diabetic and nondiabetic obese men. Diabetes Care, 33(6), 1186-1192. PubMed ↩
-
Yassin, A. A., & Saad, F. (2017). Testosterone Deficiency and Testosterone Treatment in Older Men. Gerontology, 63(2), 144–156. PubMed ↩
-
Khaw, K. T., Dowsett, M., Folkerd, E., Bingham, S., Wareham, N., Luben, R., ... & Day, N. (2007). Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men. Circulation, 116(23), 2694-2701. PubMed ↩
-
Traish, A. M., Saad, F., & Guay, A. (2009). The dark side of testosterone deficiency: I. Metabolic syndrome and erectile dysfunction. Journal of Andrology, 30(1), 10-22. PubMed ↩
-
Orwoll, E., Lambert, L. C., Marshall, L. M., Phipps, K., Blank, J., Barrett-Connor, E., ... & Cummings, S. (2006). Testosterone and estradiol among older men. The Journal of Clinical Endocrinology & Metabolism, 91(4), 1336-1344. PubMed ↩
-
Vlachopoulos, C., Ioakeimidis, N., Miner, M., & Aggelis, A. (2014). Testosterone deficiency: a determinant of aortic stiffness in men. Atherosclerosis, 233(1), 278-283. PubMed ↩
-
Carrero, J. J., Qureshi, A. R., Parini, P., Arver, S., Lindholm, B., Bárány, P., ... & Stenvinkel, P. (2009). Low serum testosterone increases mortality risk among male dialysis patients. Journal of the American Society of Nephrology, 20(3), 613-620. PubMed ↩
-
O'Connor, D. B., Lee, D. M., Corona, G., Forti, G., Tajar, A., O'Neill, T. W., ... & EMAS Study Group. (2011). The relationships between sex hormones and sexual function in middle-aged and older European men. The Journal of Clinical Endocrinology & Metabolism, 96(10), E1577-E1587. PubMed ↩
-
Malkin, C. J., Pugh, P. J., Jones, R. D., Kapoor, D., Channer, K. S., & Jones, T. H. (2004). The effect of testosterone replacement on endogenous inflammatory cytokines and lipid profiles in hypogonadal men. The Journal of Clinical Endocrinology & Metabolism, 89(7), 3313-3318. PubMed ↩





