Thyroid Lab Tests Types and Controversies
Thyroid Labs : Is TSH the Best Way to Measure Thyroid Function?
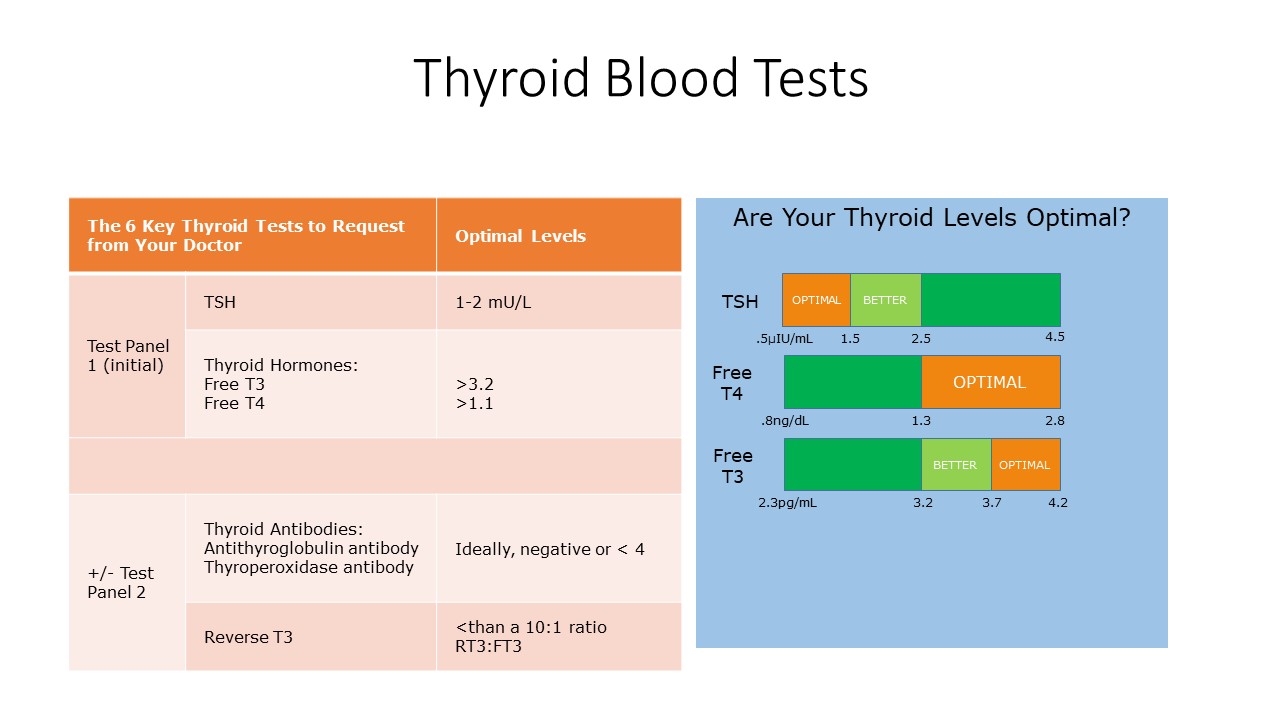
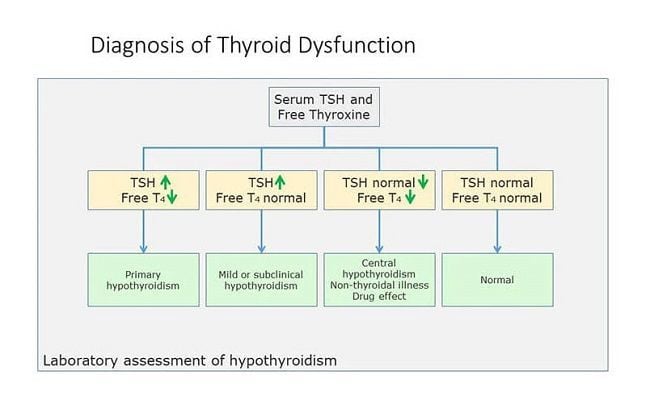
The first signs of thyroid disorder are typically related to symptoms like fatigue, weight gain, cold intolerance, hair loss, sexual dysfunction, etc. and blood screening of Thyroid Stimulating Hormone (TSH) with other thyroid hormone biomarkers, including free thyroxine (T4), is necessary to assess thyroid function. This includes testing for specific thyroid health conditions such as underactive thyroid (hypothyroidism) and overactive thyroid (hyperthyroidism), also known as thyroid conditions. Unfortunately, some physicians only measure TSH as a way to diagnose low or high thyroid function. Even though some guidelines suggest a TSH range of 0.4–4.5 micro IU/mL, some patients may be experiencing hypothyroidism symptoms at TSH levels above 3 due to occult Hashimoto’s disease or other issues, so it is always a good idea to perform a thyroid panel that includes not only TSH but also free T3 and free T4. There is ongoing controversy about whether reliance on the TSH test—to the exclusion of clinical symptoms and other tests such as Free T4, Free T3, and antibody tests—is medically sound. That is a controversy that is unlikely to be decided for years. The situation today, however, is that the majority of physicians do rely almost exclusively on the TSH test to detect thyroid disease and monitor the effectiveness of treatment, which may not always accurately reflect the levels of enough thyroid hormone in the body. Additionally, weight loss is a common symptom of hyperthyroidism, making it important to consider when assessing thyroid function.
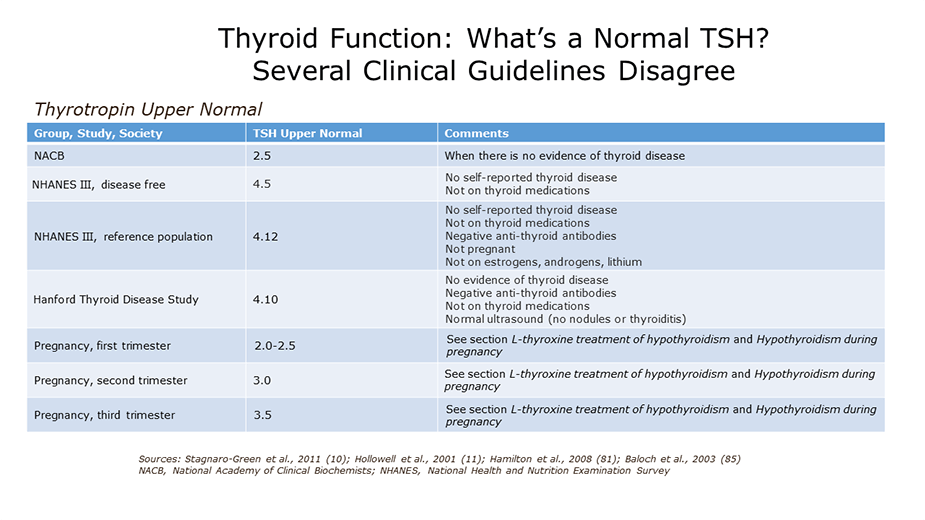
What is the Optimal TSH Range?
Since 2003, the American Association of Clinical Endocrinologists has recommended that the normal range for TSH run from 0.3 to 3.0, versus the older range of 0.5 to 4.5. So, according to the new standards, levels above 3.0 are evidence of possible hypothyroidism, and levels below 0.3 are evidence of possible hyperthyroidism. However, there is disagreement among practitioners, and some follow the older range, while others use the newer range.
An important thing to understand about TSH is that it is an inverse number when thinking about thyroid function. The higher it is, the more sluggish, underachieving and, generally, slow your thyroid is, indicating a lack of thyroid hormone. The lower it is, the more hyperactive, overachieving and, generally doing too much your thyroid, indicating an excess of thyroid hormone. Put another way: High TSH = hypothyroid, Low TSH = hyperthyroid. It is important to keep your TSH levels within the optimum range, as determined by your healthcare provider, to ensure proper thyroid hormone levels and overall health, including body temperature regulation. This small, butterfly-shaped gland, known as the pituitary gland, is located in the front of your neck and plays a crucial role in controlling your body's most important functions.
TSH levels increase as T4 levels drop, and TSH levels decrease as T4 levels rise. The reason this is the most popular test in today’s medical model is that the only treatment offered for thyroid dysfunction is thyroid hormone replacement, specifically the medicine levothyroxine, and that’s what doctors are checking when they test your TSH.
A TSH test alone doesn’t give you information about thyroid-pituitary communication, about T4 to T3 conversion in other parts of the body or about whether or not your immune system is attacking your thyroid. One important thing for people with the thyroid autoimmune Hashimoto disease to understand is that some antibodies can inhibit thyroid function by turning off instead of stimulating TSH receptors on cells. In this case, you will see high TSH and high thyroid antibodies, as well as nodules, which can be detected through thyroid antibody tests and thyroid imaging, such as a thyroid ultrasound. These tests are crucial in diagnosing autoimmune disorders like Graves’ disease or Hashimoto’s disease, and learning more about the optimum TSH range through resources such as the Thyroid Function Tests provided by the American Thyroid Association.
What are Thyroid Stimulating Hormone (TSH) and Other Thyroid Labs?
· TSH is used as a first line screening tool to assess thyroid disease. Additionally, health care providers check TSH to monitor disease progression and treatment
· TSH is high in primary hypothyroidism
· Low TSH occurs in hyperthyroidism
· Evaluation of therapy in hypothyroid patients receiving various thyroid hormone preparations, although free T3 should also be evaluated along with patient’s symptoms
· Range: 0.450−4.500 μIU/mL (>10 yr old). This range is in debate.
· Methodology: Electrochemiluminescence immunoassay (ECLIA)
T4 (Thyroxine), Total, Serum
· Used for the diagnosis of hypothyroidism and hyperthyroidism
· Free T4 is usually preferred instead of measuring total T4.
· Reference Range: 4.5–12.0 μg/dL
· Most physicians order serum free T4 instead of serum total T4
· Free T4 will provide a better evaluation of bioavailable thyroxine since it tests hormone that is not bound by proteins
T4 (Thyroxine), Free, Serum
The free T4 (FT4) assay measures the concentration of free thyroxine, the only biologically active fraction, in the serum (about 0.05% of the total T4). Free thyroxine is not affected by changes in concentrations of binding proteins such as TBG and thyroid binding prealbumin. Thus, such conditions as pregnancy, or estrogen and androgen therapy do not affect the FT4. Thus the FT4 assays generally are considered to provide the more reliable indication of true thyroid status because only the free hormone is physiologically active. In developing hypothyroidism, T4 (free T4) is the more sensitive indicator of developing disease than is T3 (Free T3), and is therefore preferred for confirming hypothyroidism that has already been suggested by an elevated TSH result.
· Measurement of circulating thyroxine not bound to proteins (TBP)
· Reference Interval: 0.82–1.77 ng/dl (>19 years old)
· The thyroid gland produces and secretes T4, otherwise known as thyroxine. Proteins bind to T4 and carry it throughout the bloodstream.
· Once in the tissues, T4 is released from the proteins and is now free to convert into the more active form called T3.
· Many physicians believe that measuring free T4 is a more sensitive test for thyroid hormone production
Reverse T3 (Triiodothyronine), Serum
· LabCorp Reference Range: 9.2–24 ng/dL
· Methodology: Liquid chromatography/tandem mass spectrometry (LC/MS-MS)
· The reverse T3 level tends to follow the T4 level: low in hypothyroidism and high in hyperthyroidism
· Increased levels of rT3 have been observed in starvation, anorexia nervosa, severe trauma and hemorrhagic shock, hepatic dysfunction, postoperative states, severe infection, and in burn patients (i.e., "sick euthyroid" syndrome)
· This appears to be the result of switchover in deiodination functions, with the conversion of T4 to rT3 being favored over the production of T3
· The Journal of Clinical Endocrinology & Metabolism states that “the T3/rT3 ratio is the most useful marker for tissue hypothyroidism and as a marker of diminished cellular functioning.”
T3 (Triiodothyronine), Total, Serum
· Second-order testing for hyperthyroidism in patients with low thyroid-stimulating hormone values and normal thyroxine levels
· Diagnosis of triiodothyronine toxicosis
· Triiodothyronine (T3) values >200 ng/dL in adults or > age related cutoffs in children are consistent with hyperthyroidism or increased thyroid hormone-binding proteins.
· In hypothyroidism, T4 and T3 levels are decreased. T3 levels are frequently low in sick or hospitalized euthyroid patients.
· Total Triiodothyronine (T3) is not considered a reliable marker for hypothyroidism.
· Free T3 is usually preferred instead of total T3 to provide a better evaluation of bioavailable triiodothyronine
T3 (Triiodothyronine), Free, Serum
The total T3 test measures the concentration of triiodothyronine in the serum. The T3 is increased in almost all cases of hyperthyroidism and usually goes up before the T4 does. As a result, T3 levels are preferable to total T4 levels for confirming hyperthyroidism that a suppressed TSH result has already suggested. T3 tests can also help rule out T3 thyrotoxicosis, a type of hyperthyroidism that shows up with T3 levels that are too high and TSH levels that are too low, while T4 levels stay within normal (euthyroid) limits. In hypothyroidism, the T3 is often normal, even when the T4 is low. Inderal steroids are just a few of the medications that have an impact on the T3, which decreases during acute illness and starvation. This test measures both bound and free hormones, including iodine, which is crucial for the production of thyroid hormones. And only the free hormone is biologically active. Since free T3 accounts for only about 0.5% of the total T3, measurement of free hormone is generally considered to provide a more reliable indication of true thyroid status. As noted above for T4 levels, anything which affects thyroid binding globulin (TBG) or albumin will affect the total T3 levels. Additionally, a radioactive iodine uptake test, also known as a thyroid uptake test, may be used to check thyroid function and diagnose hyperthyroidism.
This test quantifies the amount of free T3—that is, T3 that is not protein-bound and accessible to tissues—in the body.
· Many doctors believe that evaluating the levels of free T3 is the best indicator of thyroid function
· Needed to determine the level of active thyroid hormone primarily responsible for regulating metabolism to fuel all cellular functions
· Reference Interval: 2.0−4.4 pg/ml (>19 yr old)
Thyroglobulin Antibody and Thyroglobulin
· Measures antithyroglobulin antibodies that are commonly present in patients with Hashimoto's thyroiditis
· Antibodies against the protein thyroglobulin can destroy thyroid cells. This destruction can lead to hypothyroidism
· The test will identify the positive or negative presence of antibodies with reflex to confirm the accuracy
· Usually ordered as part of a comprehensive thyroid panel when thyroid hormone deficiency is present with no conclusive diagnosis
· Methodology: TgAb: Beckman Coulter immunometric assay, with either of the following methodologies used for reflex confirmation: Tg-IMA: Beckman Coulter immunometric assay; Tg: Liquid chromatography/tandem mass spectrometry (LC/MS-MS)
Thyroid Peroxidase (TPO) Antibodies
· Differential diagnosis of hypothyroidism and thyroiditis
The most accurate way to find autoimmune thyroid diseases like Hashimoto's thyroiditis, idiopathic myxedema, and Graves disease is to measure TPO antibody levels. Most people who have these disorders have levels of anti-TPO antibodies that can be detected.
· The highest TPO antibody levels are observed in patients suffering from Hashimoto thyroiditis. In this disease, the prevalence of TPO antibodies is about 90%, confirming the autoimmune origin of the disease
· autoantibodies also frequently occur (60%–80%) in the course of Graves disease
· Should be used in conjunction with antithyroglobulin test, since autoimmune thyroiditis may demonstrate a response to antigens other than thyroid microsomes
· Range: 0-34 IU/ML (>19 years old)
Thyroxine-binding Globulin (TBG Lab Test), Serum
· Abnormal levels (high or low) of thyroid hormone-binding proteins (primarily albumin and thyroid-binding globulin) may cause abnormal T3 concentrations in euthyroid patients
· Range: 13–39 ug/mL (>19 years old)
· Methodology: Immunochemiluminometric assay (ICMA)
BUY A COMPLETE THYROID PANEL WITH ANTIBODIES HERE
Citations:
- Demystifying Thyroid Supplementation
- Thyroid Function Tests and Risk of Alzheimer Disease: The Rotterdam Study
- Thyroid Function and Mortality: The Rotterdam Study
- Thyroid Testing Best Practices: Reverse That Order for Reverse T3
- Thyroid Function and the Risk of Alzheimer Disease: A Population-Based Study
- Thyroid Hormone Therapy: New Insights and Approaches