CBC with Differential

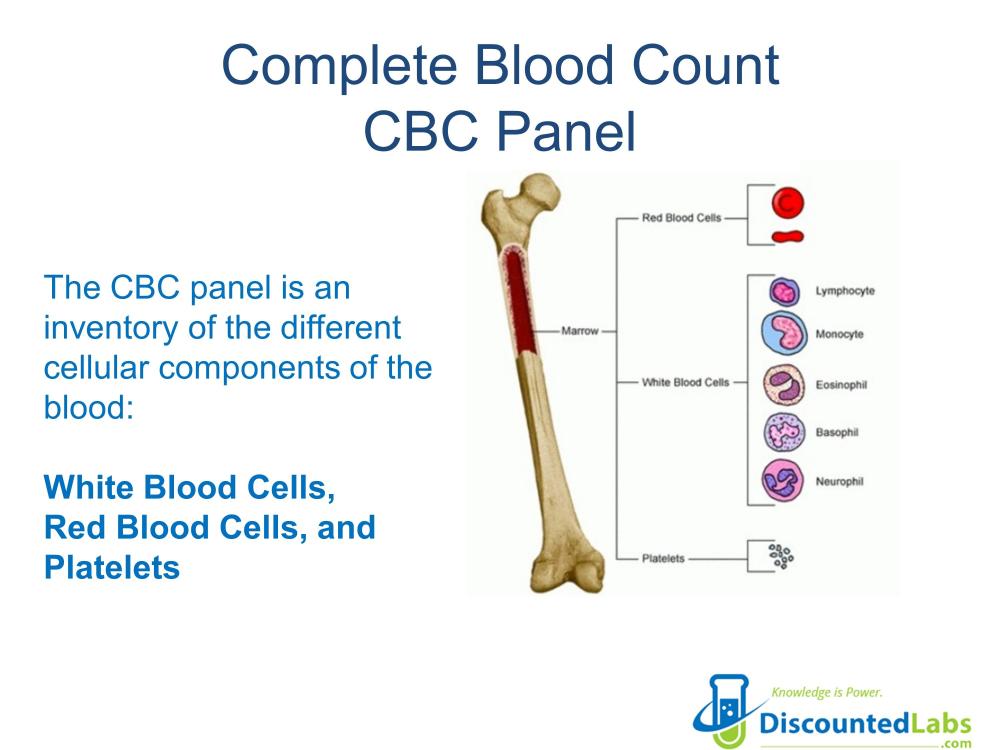
A complete blood count CBC with differential test panel measures several components of your blood including:Red blood cells, which carry oxygen, White blood cells, which fight infection, Hemoglobin, the oxygen-carrying protein in red blood cells, Hematocrit, the proportion of red blood cells to the fluid component in your blood (which correlated with blood thickness), and Platelets, which help with blood clotting. This is also called Complete Blood Count (CBC) with Differential and Platelets Blood Test
A complete blood count (CBC) with a differential tests several parts of your blood. It checks:
- red blood cells, which carry oxygen.
- White blood cells, which fight infections.
- Hemoglobin, the protein in red blood cells that carries oxygen.
- Hematocrit, which shows the ratio of red blood cells to fluid in your blood. This tells how thick your blood is.
- Platelets, which are crucial for blood clotting.
Some people refer to this test as the Complete Blood Count (CBC) with Differential and Platelet Blood Test.
Discounted Labs: CBC with Differential Test Guide
What is the purpose of conducting a CBC with differential testing?
A CBC with differential test shows important information about different types of blood cells. This includes white blood cells, red blood cells, and platelets. The test helps doctors discover health issues like infections, anemia, and leukemia. It does this by checking the number and health of these blood cells.
A complete blood count (CBC) with a differential test checks different parts of your blood. It looks at the amount of red blood cells. These cells carry oxygen to your body. The test also measures white blood cells, which help your body fight infections. Hemoglobin is checked as well. Hemoglobin is the protein in red blood cells that carries oxygen. The test measures hematocrit too. Hematocrit shows the ratio of red blood cells to the liquid part of your blood. This shows how thick your blood is. Finally, it checks platelets, which are important for blood clotting.
CBC with Differential: Understanding Key Insights
A complete blood count (CBC) with differential checks several parts of your blood. It looks at white blood cells, red blood cell (RBC) count, hemoglobin, hematocrit, and platelets. This test is very important. A CBC provides helpful information about your overall health. It can detect issues like anemia, infection, and leukemia. A CBC with differential is one of the most common laboratory tests done today. It shows how many blood cells you have. It also examines how well your red blood cells carry oxygen by looking at rbc indices, hemoglobin, and hematocrit.
This CBC with Differential Panel Includes
Tests included:
- White blood cell count (WBC or leukocyte count)
- Differential count of white blood cells
Red blood cell count (RBC or erythrocyte count)
- hematocrit (hct)
- Hemoglobin (Hbg)
- mean corpuscular volume (MCV)
- mean corpuscular hemoglobin (MCH)
- Mean corpuscular hemoglobin concentration (MCHC)
- Red cell distribution width (RDW)
- Count of platelets
- Mean platelet volume (MPV)
Complete Blood Count: CBC Blood Test Panel
Whole blood contains different types of cells floating in a liquid called plasma. A complete blood count (CBC) or full blood count (FBC) looks at these cells, including red blood cells, white blood cells, and platelets. The CBC provides valuable information about your overall health. Healthcare workers use it to find and understand several health problems, like anemia, infections, and blood issues. The National Cancer Institute in Bethesda explains that a complete blood count measures these blood cells. The counts from the small sample taken during the CBC are usually displayed as the number of cells in one cubic millimeter of blood (cells/mm3) or as a percentage of all blood cells.
Red Blood Cells
Red blood cells, or erythrocytes, carry oxygen from the lungs to body cells. They use a molecule named hemoglobin for this job. Anemia happens when there are not enough red blood cells. This condition can leave a person feeling tired, weak, and short of breath. There are several tests to find out different types of anemia.
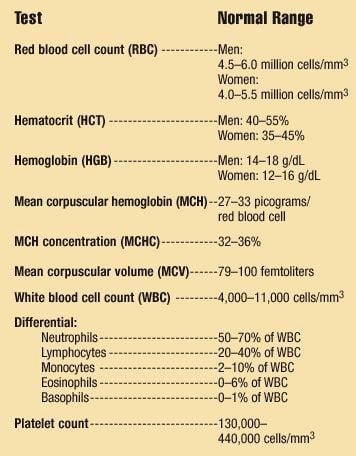
Red Blood Cell Count (RBC) :
The number of red blood cells in the blood is known as the red blood cell count. For men, the normal range is 4.5–6.0 million cells/mm³. For women, it is 4.0–5.5 million cells/mm³. Women often have lower counts compared to men. This is mostly due to blood loss during their period.
Hematocrit (HCT) :
This test checks how many red blood cells (RBCs) are in your blood. It tells you the percentage of red blood cells compared to all the blood volume. A normal hematocrit level for men is between 40% and 55%. For women, it is between 35% and 45%. A hematocrit test can help find anemia and other issues. These issues may include liver disease, bleeding problems, or how well red blood cells are made. Hematocrit levels can increase if you adapt to higher altitudes or if you are dehydrated. Typically, women have lower levels than men. Some men taking testosterone might have higher hematocrit. This can be managed with the right checks.
Hemoglobin (HGB) :
Hemoglobin is measured in grams per deciliter (g/dL) of blood. In healthy adults, men typically have between 14 and 18 g/dL of hemoglobin. Women usually have between 12 and 16 g/dL. A simple rule is that hemoglobin should be about one-third of the hematocrit. Hemoglobin is a protein that contains iron and is found in red blood cells (RBCs). It allows these cells to carry oxygen and carbon dioxide through the blood. Checking hemoglobin levels shows how well your blood can transport oxygen to all the cells in your body. A lower level may indicate anemia. Hemoglobin levels can increase when people adjust to high altitudes. Generally, women have lower hemoglobin levels than men.
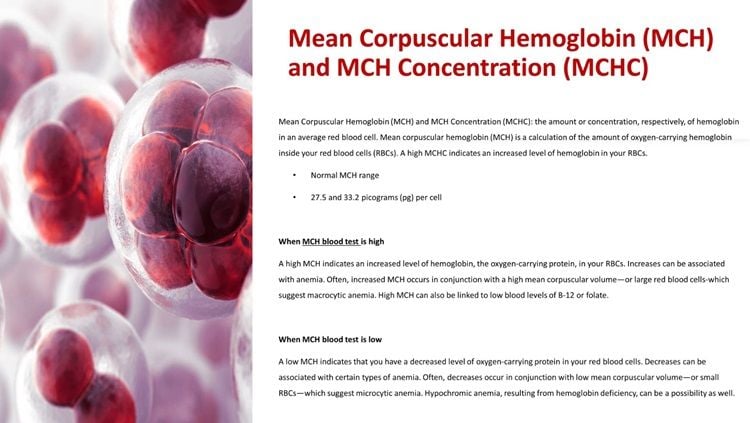
Mean corpuscular hemoglobin (MCH) and MCH concentration (MCHC ) :
Mean corpuscular hemoglobin (MCH) measures how much hemoglobin is inside an average red blood cell. Hemoglobin carries oxygen, which is important for your body. A high MCH means there is more hemoglobin in your red blood cells (RBCs). This can happen when someone has anemia. A bigger mean corpuscular volume, which means larger red blood cells, usually pairs with higher MCH. This may indicate macrocytic anemia.
In contrast, a low MCH shows there is less hemoglobin in your red blood cells. A drop in MCH is often linked to certain types of anemia. A low MCH usually occurs with a low mean corpuscular volume, which means your RBCs are smaller. This suggests microcytic anemia. A lack of hemoglobin can also lead to hypochromic anemia.
The mean corpuscular hemoglobin concentration (MCHC) tells us how much hemoglobin each red blood cell (RBC) has. A high MCHC means there is a lot of hemoglobin in your RBCs. This is often seen as a high RBC count. A high MCHC is usually more about technical issues than health problems. Problems during collection, transport, or storage of the blood sample can change the shape of your RBCs. This can lead to a high MCHC reading. A low MCHC means there is less hemoglobin in your RBCs. A drop in MCHC can be linked to certain types of anemia. This includes issues like iron deficiency or thalassemia, which is a genetic disorder.
Mean Corpuscular Volume (MCV):
The size of your red blood cells can change. The mean corpuscular volume (MCV) shows the average size of your red blood cells (RBCs). A high MCV means your RBCs are larger, known as macrocytic. This can occur if you have certain types of anemia or do not get enough vitamin B12 or folic acid. A low MCV means your red blood cells are smaller, called microcytic. A low MCV can indicate that you have anemia as well. Common reasons for low MCV include iron deficiency, chronic illness, thalassemia, or low amounts of RBCs. When your iron is low, red blood cells may be smaller. Some vitamin shortages or certain medications can cause cells to be larger than normal. In your CBC report, look for two columns: "reference range” and your results. If your results are within the reference range, they are normal. If they are higher or lower, this means they are abnormal. Mild anemia is a common reason for these unusual results.
Red Blood Cell Distribution Width (RDW):
A method to check the size and uniformity of red blood cells.
White Blood Cells
White blood cells (WBCs) are important for keeping your body safe. There are five types of WBCs. Each type has a unique role that helps fight illness or injury.
White blood cells, or leukocytes, play an important role in keeping the body safe from infections. A CBC measures the number of different types of white blood cells.
White Blood Cell Count (WBC) :
The total number of white blood cells in the body is called the white blood cell count (WBC). This count is important for checking how healthy the immune system is. A healthy adult usually has about 4,000 to 11,000 white blood cells in one cubic millimeter of blood. A high white blood cell count, which is also known as leukocytosis, can occur due to infections, inflammation, or stress on the body. Some diseases, like myeloproliferative and lymphoproliferative disorders, can also cause a high count. A high white blood cell count means a person is fighting an infection or has inflammation. On the other hand, a low white blood cell count, called leukopenia, may indicate problems like an autoimmune disease, issues with bone marrow, or certain types of cancer. It is important to monitor any large changes in the white blood cell count. This can help find the cause and guide the right treatment.
Differential: A report lists the percentages of different types of white blood cells in relation to the total number of white cells. You can find the actual counts by multiplying these percentages with the total number of white blood cells (WBC).
Neutrophils:
A neutrophil is a kind of cell that helps our body fight bacterial infections. These cells are the most common type of white blood cell. Neutrophils usually make up about 50 to 70% of all white blood cells in our body. If the count of neutrophils drops below 500 to 750 cells/mm3, the risk of getting a bacterial infection increases. Neutrophils are very important for the immune system, human services, and medicine. They respond to bacterial infections and swelling. When they do, neutrophils move out of the blood vessels to the infection sites. The main cells found in pus from a wound are neutrophils.
Lymphocytes:
There are two main types of lymphocytes. B cells make antibodies to fight invaders in the body. T cells focus on infected or cancer cells and help manage the immune system. Lymphocytes usually make up about 20-40% of all white blood cells. They are the second most common type of white blood cell.
Lymphocytes can be divided into larger natural killer cells and smaller B and T lymphocytes. Natural killer cells are important for our immune system. They help protect us from tumors and viral infections. They respond to changes on tumor cells and infected cells.
B and T lymphocytes react to infected cells in different ways. T lymphocytes use a cellular response, while B lymphocytes use antibodies. Some T cells can attack and destroy your own infected or cancerous cells.
Monocytes:
Monocytes are cells that help fight germs. They do this by swallowing and destroying these germs. Monocytes stay in your blood for about 24 hours. After that, they leave the blood and move into the tissues. In the tissues, they grow into bigger cells called macrophages. Monocytes and macrophages usually make up 2-10% of all white blood cells.
Like other white blood cells, monocytes start in the bone marrow. This is the soft part inside bigger bones. They can eat harmful invaders by using a process named phagocytosis. Monocytes also help kill infected cells. Additionally, they play a role in a condition called atherosclerosis. This condition affects our arteries and can lead to heart disease and stroke.
Eosinophils:
Eosinophils are special cells in our body. They help us fight off parasites and allergic reactions. These cells belong to our immune system. Eosinophils make up about 0-6% of all white blood cells. Together with basophils and mast cells, they are important in managing allergies and asthma.
Basophils:
Another type of cell involved in allergic reactions is histamine. It makes up one percent or less of all white blood cells. Basophils are the rarest kind of the five types of white blood cells. When they activate, basophils release several substances. These include histamine and interleukin-4. Both substances play important roles in the allergic response.
Platelets
Platelets, or thrombocytes, are small cells that help with blood clotting. A healthy platelet count is about 130,000 to 440,000 cells per mm3. If your platelet count is low, known as thrombocytopenia, you could bruise easily and bleed more than usual. This condition can be caused by some medications, autoimmune reactions, spleen damage, or certain immune diseases.
Platelets play an important role in stopping bleeding when you get hurt. They gather at the injury site and seal the area of the bleeding vessel. They also help blood clot more quickly. A doctor may check your platelet count if you often bruise or before surgery. Your count can change because of bleeding disorders, heart disease, diabetes, or inflammation.
Thrombocytosis is when your platelet count is high. This can occur due to inflammation, injury, or iron deficiency. In some rare cases, like essential thrombocythemia, platelet counts can become very high. When there are too many platelets, it is called thrombocytosis. This condition can raise the risk of heart issues caused by blood clots.
MPV
Mean Platelet Volume shows how big your platelets are. The width of platelets can shift as they get older. New platelets are larger than the older ones.
Preparing for Your CBC Test
When you prepare for a complete blood count (CBC) test, you don’t need to change much in your daily life. It's still very important to follow any specific instructions from your healthcare provider. A blood sample will be taken from a vein in your arm using a small needle. This moment might feel like a quick sting. It’s a good idea to drink plenty of water before the test. Being well-hydrated helps your healthcare provider get a better blood sample from the vein. If there are additional tests with the CBC, your healthcare provider will let you know how to prepare for those too.
If your healthcare provider wants you to fast for tests, they will let you know how long to fast before they take your blood sample. Normally, you don't have to skip food or drinks just for the CBC test. You should feel free to talk to your healthcare provider about any questions or concerns you have about the procedure. This will help make your testing experience better.
How to Prepare for a CBC Test
Preparing for a CBC test is simple and usually requires a few steps. First, inform your healthcare provider, including your MD, about any medications you are taking. Some medications can affect the results of your blood test. Normally, you do not need to fast for a CBC. However, if you have other tests at the same time, fasting might be necessary. It is a good idea to drink enough water before your appointment. This can make the blood draw easier by increasing your blood volume.
On the day of the test, wear a short-sleeved shirt or clothing that makes it easy for your healthcare provider to reach your arm. This will help them collect your blood sample more easily. When they take your blood, you may feel a small pinch, but it will be quick, usually taking less than five minutes. After they collect the blood sample, your healthcare provider will put on a bandage to help reduce any bruising.
It is really important to follow any extra instructions from your healthcare provider. These instructions can change based on your health needs. They might also be different if you are having several tests done.
Understanding CBC Test Results
Once your blood sample is tested, your healthcare provider will discuss the results with you. A CBC test can reveal several issues. This includes abnormal results such as anemia, infections, and various blood disorders. The test results typically show the counts of red blood cells, white blood cells, hemoglobin, hematocrit, and platelets. Each of these numbers helps you understand more about your overall health.
Abnormal results can show that there might be health issues. It's important to understand what these numbers mean for you. For instance, a low red blood cell count could indicate anemia. A high white blood cell count may suggest an infection, inflammation, or lymphoma. If your results fall outside the normal ranges, your healthcare provider will talk with you about what steps to take next. This may involve conducting additional tests or closely monitoring your health.
Interpreting Normal and Abnormal CBC Counts
Interpreting CBC results means understanding the normal ranges for different parts of the blood. For adults, the white blood cell count is typically between 4,000 and 10,000 cells/mm³. Men usually have between 4.5 and 6 million red blood cells per mm³. Women usually have between 4.0 and 5.5 million red blood cells per mm³. If the results are not normal, they can show different health problems. A high white blood cell count might suggest an infection. A low platelet count might mean a higher risk of bleeding.
Healthcare providers will review your complete medical history and any symptoms you have when they analyze these results. It is important to discuss any strange findings with your provider. Talking openly about these issues can help you understand what they might mean for your health. Regular CBC tests are a key part of a routine exam. They can help manage ongoing health problems and make sure you get the care you need on time.
Summary
In conclusion, knowing the results of a CBC with differential test can give important clues about a patient's overall health. This test can help find several conditions, including those related to cancer treatment. By looking at key parts of the test, such as the white blood cell count and differential count, doctors can learn more about possible health issues. This knowledge helps them make better treatment plans for cancer patients. It is vital for both patients and healthcare providers to understand what these test results mean. They need to work together to address any concerns, especially for the upcoming appointments in October related to cancer treatment.
Commonly Asked Questions
What diseases can be diagnosed with a CBC?
A Complete Blood Count (CBC) is a common blood test that provides important information about the types and numbers of cells in your blood. It can help diagnose a variety of conditions, including:
1. Anemia
2. Infections
3. Leukemia
4. Bleeding disorders
5. Inflammatory conditions
A CBC is a valuable tool for healthcare providers to assess your overall health and to diagnose a wide range of diseases and conditions based on the results of the test. It is often one of the first tests ordered in a routine check-up or when evaluating symptoms that could indicate an underlying health issue.
Can the results of a CBC with Differential test vary depending on the individual's age or gender?
The results of a Complete Blood Count (CBC) with Differential test can indeed vary depending on the individual's age and gender. For example, certain values such as hemoglobin levels may differ between males and females due to physiological differences. Additionally, age-related changes in blood cell counts can impact the interpretation of the test results. It is important for healthcare providers to consider these factors when analyzing CBC with Differential test results to ensure accurate diagnosis and appropriate treatment plans tailored to each individual's specific health needs.
References:
Complete Blood Count (CBC): What to Know - MedlinePlus
Complete Blood Cell Count (CBC) with Differential – Mayo Clinic Pediatric Catalog
Complete Blood Count (CBC): Purpose, Procedure, and Results - Cleveland Clinic
What Is a Differential Blood Count? - WebMD
Complete Blood Count (CBC) with Differential, Reflex to Peripheral Smear Review - Labcorp
Understanding the Complete Blood Count with Differential - PubMed
Blood Differential Test: Purpose, Procedure, and Results - Mount Sinai
How to Read Blood Test Results - Cancer Treatment Centers of America
Complete Blood Count (CBC): Definition, Normal Ranges, and Results - Sight Diagnostics
Complete Blood Count with Differential: Purpose and Results - URMC Health Encyclopedia
HOW DOES DISCOUNTEDLABS.COM WORK?
-
Go to the "Find a Location" page to find the closest lab location. No need to make an appointment since walk-ins are welcomed. Once you have identified your closest location, go to step 2.
-
Go to "Choose a Test" and add your selection (s) in the shopping cart. If you prefer to save money on bundled tests, we have created "Lab Test Panels" that can help you decide what to order.
-
If you have a discount coupon code, add it to your cart.
-
A $8 lab processing fee will be added to your total.
-
Pay using a credit card.
-
You will receive an order confirmation and instructions email on how to download your lab request.
-
Print lab request form that you downloaded.
-
Take that form to the closest location. Get your blood drawn.
-
You will receive an email when the results are ready for you to download.
Note: You cannot place an order under someone else's profile. The profile person's name will appear on the lab order form.If you have further questions, please email [email protected].
